Three hundred and thirteen patients (123 males and 190 females) participated in the survey (mean age: 53 ± 17 years; range: 18–87 years). In Group 1 (dental location: private practice), 109 patients filled out questionnaires (mean age: 51 ± 15 years; range: 18–82 years; 24 males and 85 females). In Group 2 (dental location: healthcare system within the hospital), 104 patients filled out the questionnaires (mean age: 53 ± 18 years; range: 21-80 years; 50 males and 54 females). Group 3 (dental arrangement: within a peat private practice within the hospital) included 100 questionnaires (mean age: 54 ± 19 years; range: 19-87 years; 51 females and 49 males).
Table 1 summarizes the main socio-demographic data of the patients at baseline, divided into three different settings.
Most patients showed a BMI within the normal range (p= 0.02; Fig. 1). Group 1 had the higher number of overweight patients (n = 8), and Groups 2 and 3 showed the highest number of overweight or obese patients (n= 50 and n = 43, respectively).
Private practice Group 1 (n = 105, because four patients did not record their height and/or weight); Group 2 healthcare system within the hospital (n = 104); Group 3 private practice within the Monia within the hospital (n = 100).
Most patients in Group 1 (private practice) reported not taking medication daily (mean= 0.7 ± 1.2 medications/day; range: 0–7 medications) (Figure 2). In Group 2 (hospital healthcare system) and Group 3 (private practice within the hospital, within the Monia ), most patients had a daily intake of one or more medications (mean = 1.8 ± 2.1 medications/day with a range of 0–10 medications and mean = 1.5 ± 2.4 medications/day with a range of 0–10 medications, under rather) (Figure 2). Group 2 showed a higher number of patients taking 3 or more drugs per day (p < 0.01; Figure 2).
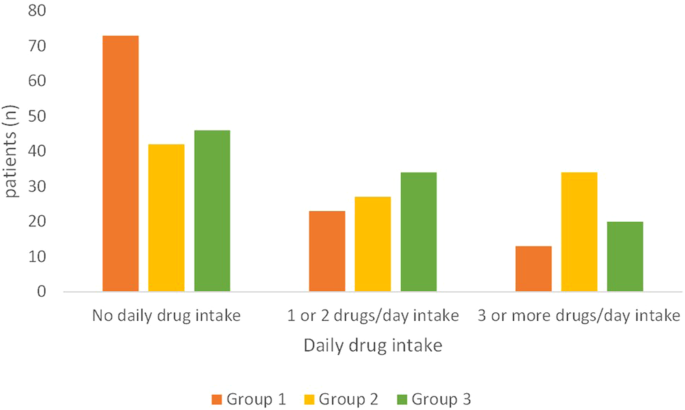
Private practice Group 1 (n = 109); Group 2 healthcare system within the hospital (n = 103, one patient reported no response); Group 3 within the Moniaprivate practice within the hospital (n= 100).
Answers to the questionnaire
“Have you ever followed a diet?”
This question provides an indication of the patient’s previous inclination and sensitivity to receive nutritional counseling. In all groups, approximately half of the patients reported following a diet: 63 patients in Group 1, 57 patients in Group 2, and 47 patients in Group 3, without significant differences (p= 0.28). In most cases, the diet was prescribed by a dietician, nutritionist, or clinician, and the diet was self-made only in a few cases (Group 1, n= 10; Group 2, n= 22; Group 3, n= 23). In Group 1, the patients who had already followed a diet were predominantly female (8 males and 38 females), while, in the other groups, the sexes were balanced.
In Group 1, 15 patients out of 63 (23.8%) who had already received a diet had a BMI outside the range: 3 of them were obese (class I n= 1; class II n= 1; class III n= 1) and 11 were overweight, and one patient was slightly overweight. Among patients who reported never receiving a diet (n= 46), a much higher number of patients (n= 21; 45.6%; p= 0.02) recorded a BMI out of range compared to the patients who were already on a diet: 10 patients were overweight, 4 were obese(class I n= 2; class IIn= 2) and 7 was slightly overweight.
In Group 2, 30 patients out of 47 (63.8%) who had already received a diet showed a BMI out of range (three of them were in class I obesity; 27 patients were overweight). They were significantly more than non-diet patients with a BMI outside the range ( n= 22 out of 57, 38.5%;p= 0.02 ;15 were overweight, five were in class I obesity, and two were slightly overweight).
In Group 3, 29 patients out of 53 (54.7%) who had already received a diet had a BMI outside the range (twenty were overweight, six were in class I obesity, two were in class II obesity, one was slightly overweight), and, among the 47 patients who had not previously received a diet, 17 of them (36.1%; p= 0.17) that BMI was out of range (twelve were overweight, two were in class I obesity, one was in class II obesity, one was slightly overweight, one was visibly underweight).
“Would you like advice on nutrition, in general and, specifically, to prevent oral diseases, such as periodontitis, tooth decay and oral cancer?”
The majority of patients (>80%) reported a willingness to receive nutrition information in all three Groups (Figure 3;p= 0.01). Among the patients who were not interested in receiving nutritional advice, two were overweight in Group 1, and, in Group 3, one was overweight and one was in class I obesity. Group 2 showed that a higher number of patients were “no different” in receiving nutritional advice.
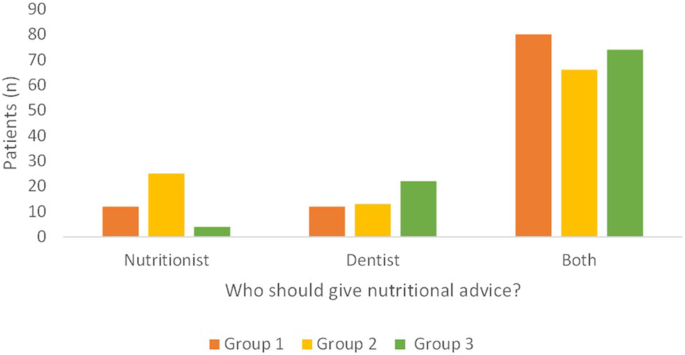
“Do you think your dentist, nutritionist or both should give you such advice?”
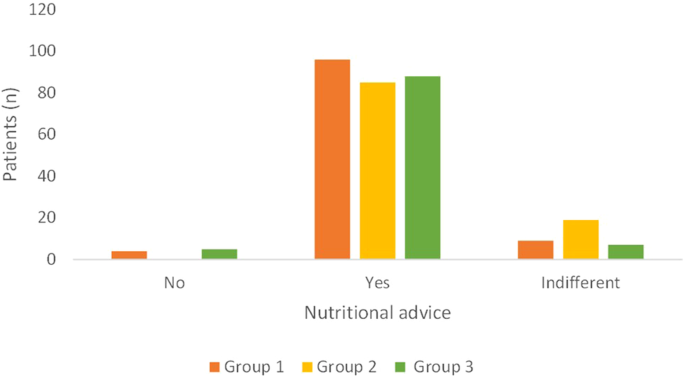
Private practice Group 1 (n= 109); Group 2 healthcare system within the hospital ( n= 104); Group 3within the Moniaprivate practice within the hospital ( n= 100).
In Group 1, 5 patients did not answer this question; therefore, only 94 responses were collected.
Most patients, in all Groups, recognized that both the dentist and the nutritionist had a role in providing advice (Figure 4; p< 0.01). In a few cases, only the role of the dentist or only the nutritionist was recognized, with no difference between the two figures for Group 1, and Group 2 recognized the role of the nutritionist more than Group 3, which reported primary importance. of the dentist (Figure 4;p= 0.0002).
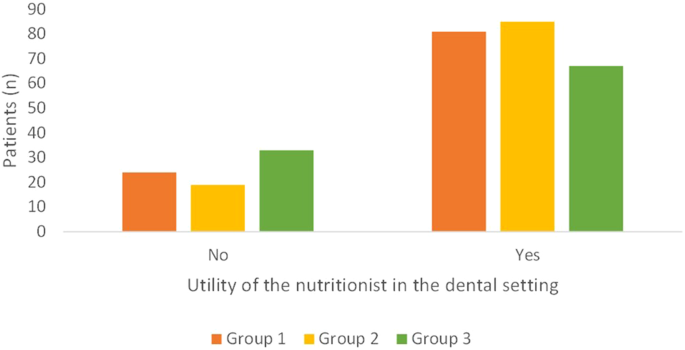
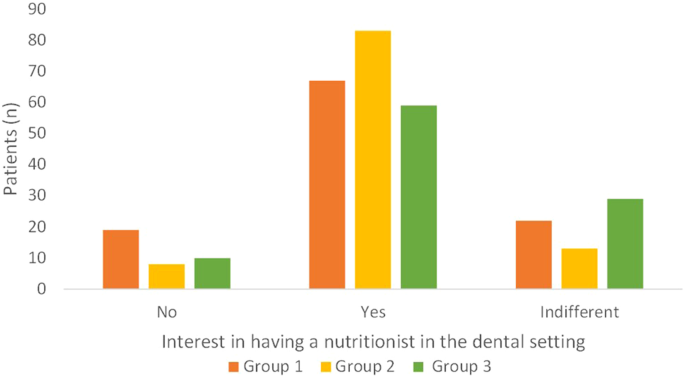
“Do you think the figure of the nutritionist can be useful in the dental clinics?”
Private practice Group 1 (n= 104, five patients reported no response); Group 2 healthcare system within the hospital ( n= 104); Group 3within the Moniaprivate practice within the hospital ( n= 100).
In all groups, the majority of patients in the dental setting considered the nutritionist useful, especially in Group 2, which had patients from the health care system (Fig. 5;p= 0.05).
“Would you be interested in having a nutritionist at the dental clinic you are referring to be able to advise on nutrition in general, providing a diet that would be useful in managing diseases other than oral diseases and prevent (systemic diseases, for example). diabetes or cardiovascular disorders)?”
Private practice Group 1 (n= 105; five patients did not answer this question); Group 2 healthcare system within the hospital ( n= 104); Group 3within the Moniaprivate practice within the hospital ( n= 100).
Most patients expressed an interest in having a nutritionist at the dental clinic they refer to (Figure 6; p< 0.01). This was much more evident in Group 2, where more than 80% of patients responded positively to this item (Figure 6;p= 0.003). Among patients who were not interested in having a nutritionist within the dental setting, 8 patients in Group 1 had a BMI outside the range (four were overweight; two were class I obese; one was obese class II; one was slightly overweight; there were 4 overweight patients in Group 2; 8 patients were in Group 3 outside or range (six were overweight; two were in class I obesity).
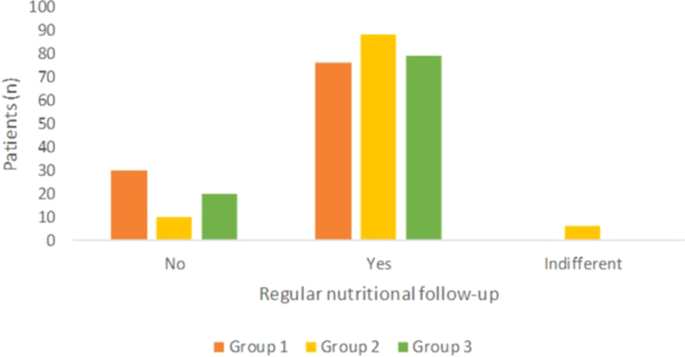
“In addition to planning a diet, do you think it would be useful to arrange a regular follow-up with the nutritionist to monitor the achievements of the dietary goals?”
Private practice Group 1 (n= 108; one patient did not answer this question); Group 2 healthcare system within the hospital ( n= 100; four patients gave no response); Group 3within the Moniaprivate practice within the hospital ( n= 100).
Most patients recognized that regular nutritional follow-up planning was valuable, especially in Group 2, where patients responded positively in more than 80% of cases. (Figure 7;p< 0.01).
Private practice Group 1 (n= 106; three patients did not answer this question); Group 2 healthcare system within the hospital ( n= 104); Group 3within a peatprivate practice within the hospital (n= 99; one patient did not answer this question).