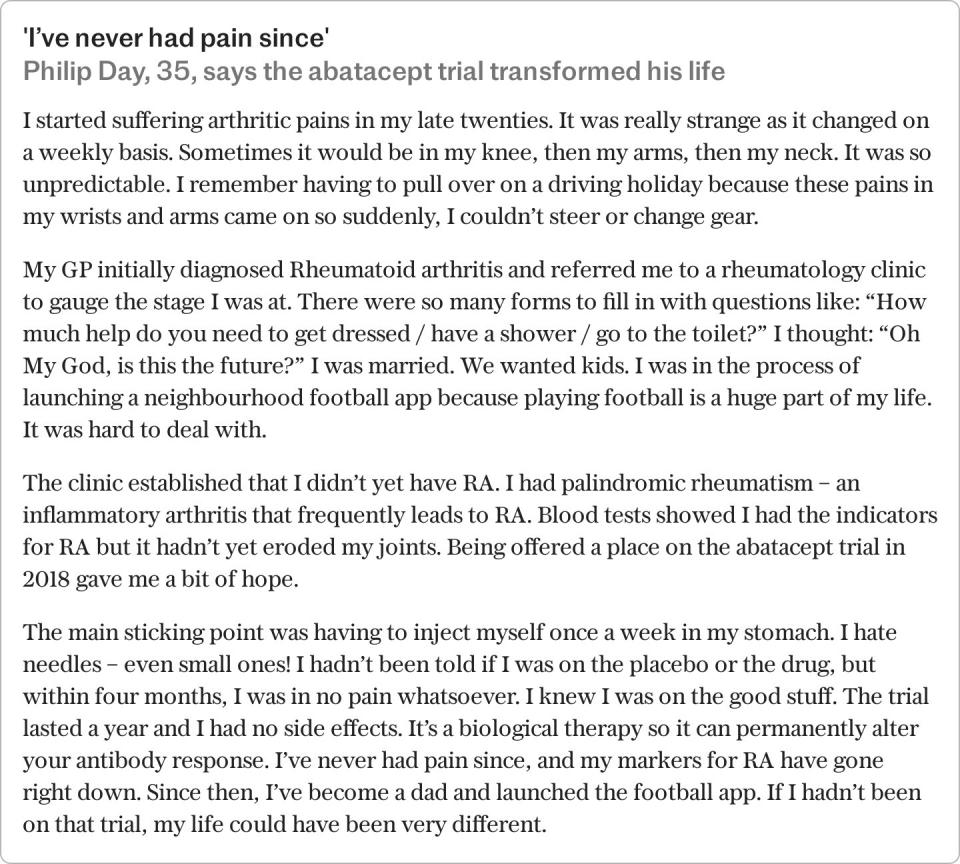
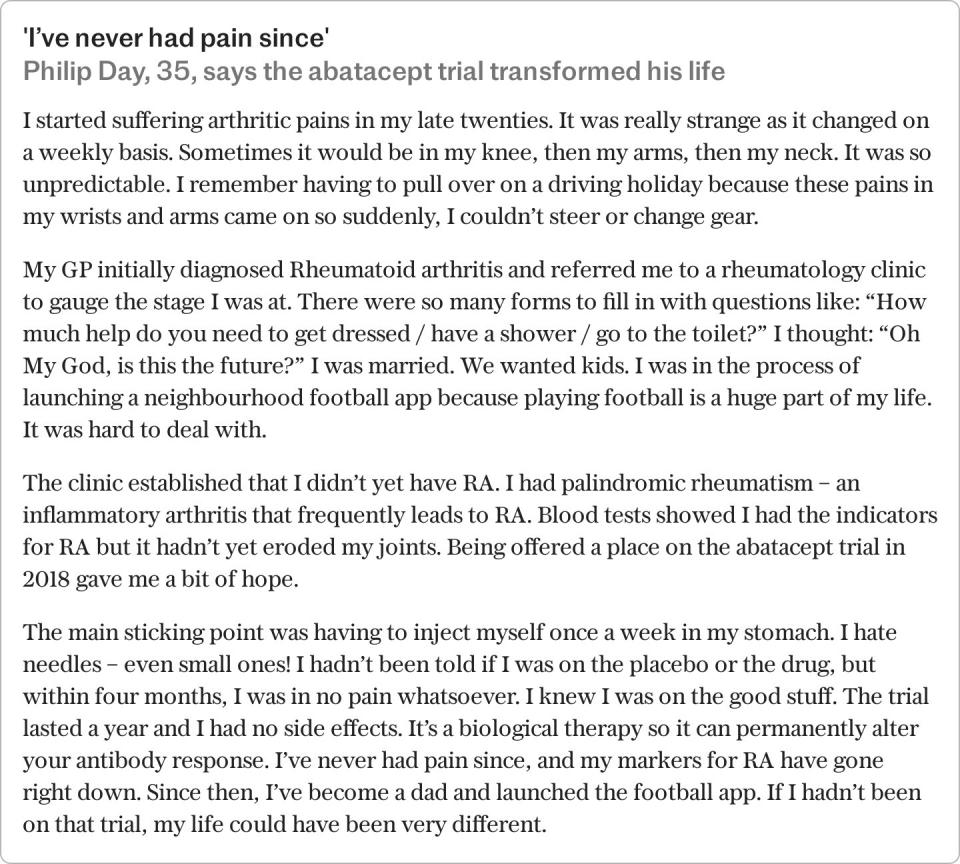
Rheumatoid arthritis is chronic, long-term and incurable, but a recent trial offers hope that it could be prevented.
The trial focused on an existing arthritis drug, abatacept, usually a second- or third-line treatment for those with well-established rheumatoid arthritis (RA). This time however, it was given to patients who had not yet developed the disease, but were considered high risk. After one year, only 6 percent had developed RA compared with 29 percent taking a placebo. It gives hope to millions.
RA is the most common form of autoimmune inflammatory arthritis, and it occurs when the immune system goes wrong, attacking our own bodies at the joints, causing hot, red, painful inflammation. Abatacept dials down the T cells involved in our immune system’s inflammatory response (a response that’s helpful when you’re fighting a pathogen, but not when it’s attacking healthy tissue). .
So who is at risk of RA, what are the symptoms and what treatment paths are currently available?
Signs and Symptoms: how does RA feel?
“Rheumatoid arthritis may sneak up on you with occasional pain in the joints of your hands or feet, or in some cases, you may wake up one morning with such stiffness and pain, you can’t move parts of you,” a says Dr. Wendy. Holden, consultant rheumatologist at Arthritis Action.
Basically, RA is swelling, stiffness, warmth, redness and pain in the joints, which is almost always worse in the morning and after long periods of rest. (This early morning stiffness and pain can last for two to three hours.) “It’s most common in the joints of the hands and feet, but you can find it in the other joints in between—the shoulders, the elbows, knees and ankles,” says Dr. Holden. “Swelling is critical. You can see it. Your fingers may look swollen. Your shoes can feel tighter. In the worst cases, without treatment, the hands can resemble boxing gloves. It can also make you very tired, lethargic and deprived of food.”
Who is most likely to develop RA?
“The peak age of onset is 46 to 70,” says Dr Benjamin Ellis, consultant rheumatologist and senior clinical adviser for Versus Arthritis. “You’re more at risk if a parent or sibling has it, and it’s more common in women.” (Women are two to three times more likely to develop RA.) If you are overweight or smoke, you are also more likely to develop RA. There is some evidence that eating a lot of red meat and not getting enough Vitamin C can also raise your risk.


What causes RA?
For baldness, we don’t know, although it is believed to be a combination of genetic and environmental factors. “RA happens when the immune system goes wrong and starts attacking the joint. No one knows the trigger, although there are many theories,” says Dr Holden. “Stress is thought to be one trigger. Another theory is that it is triggered by some infection in susceptible people.” Gum disease has been highlighted as one suspect. Another is the Epstein Barr virus. In truth, there is no solid evidence for a single trigger.
How is RA diagnosed?
Ideally, as quickly as possible. Prompt diagnosis and treatment make a big difference to the long-term prognosis. “The whole time you’re not treating RA, the immune system is attacking the joints, eating holes in the cartilage that houses the joints and once it’s gone, you can’t get it back – no the technologies we have to do. so far,” says Dr Ellis.
“National Institute for Health and Care Excellence (NICE) guidelines state that GPs should refer anyone with suspected RA to a rheumatology team within three working days and treatment should not start more than six weeks from time of referral.”
Diagnosis can be simple, says Dr Holden. “Often, the symptoms and swelling are so specific, you know as soon as a patient walks in the door. Blood tests can also give a good indication, if they reveal certain inflammatory markers and antibodies produced by the immune system called anti-CCP. We can also look for inflammation and damage within the joints through X-rays, ultrasound or, just as commonly, MRI scans.”
How serious is RA?
“At its worst, and when left untreated, it can be completely devastating, and incompatible with normal life,” says Dr Holden. Pain and inflammation can stop you from being able to work. Untreated RA can lead to permanent bone and cartilage damage, ruptured tendons and joint deformities. RA increases your risk of cardiovascular disease and certain cancers including lung and prostate, although the reasons are not clear and common risk factors such as smoking and being overweight may be involved.
Inflammation in your lungs can lead to conditions such as pleurisy, pulmonary fibrosis or chronic obstructive pulmonary disease (COPD). Depression is often a co-morbidity with RA with a prevalence two to three times higher than in the general population.
The treatment options
“The main aim of treatment is to control and rebalance the immune system,” says Dr Ellis. In recent years there have been huge advances in our ability to do this. Conventional Disease Modifiers Anti-rheumatic drugs (cDMARDs), such as low-dose methotrexate, are usually the first step, given in tablet form. They work simultaneously across many different pathways to regulate the immune system.
If trying two cDMARDs was not effective, the next step is to take biological DMARDs (bDMARDs), a more accurate tool.
“These have changed the lives of hundreds of thousands of people around the world when conventional medicine didn’t work,” says Dr Ellis. “Their genius is that they use a trick of the immune system to control the immune system itself.”
These DMARDs are artificial antibodies created in a laboratory that are administered by injection. In the most common of these, called anti-TNF therapies, the antibodies block a cytokine called TNF, the “chemical messengers” in our bodies that cause inflammation in the joints. The presence of these antibodies on the cytokines is a signal for the immune system to clear them. Most patients self-inject these antibodies at home using a pre-filled device somewhat like an EpiPen – it could be once a week, once every two weeks, monthly or even less.
“Initially, biologics were very expensive, and NICE only approved them for people with the most severe disease,” says Dr Ellis. “As costs fell, people with moderate disease were also able to access them.”
More recent ones are JAK inhibitors that work by blocking the signaling system in the white blood cells to stop them from continuing to attack the immune system.
“It’s hugely frustrating that the only way to know which treatment will work best for any given person is to try one for a bit, then if that doesn’t work try another. remove another for a bit, and so on,” says Dr Ellis. “Maybe in the future, maybe before I retire, a blood test, or a fluid test of the joint or a biopsy, will tell you what treatment you would respond to. Then we could go straight to the treatment that would work best for you.”
In addition to medication to control the progression of RA, a doctor may prescribe pain medication such as paracetamol, ibuprofen or steroids delivered by tablet or injection.
How can I manage my arthritis?
“Take your medication on schedule,” says Dr. Holden. “Once your immune system is under control, the aim will be to carefully reduce the medication with the support of your doctor and see how low you can go. In some cases, you might be able to stop it.”
Exercise is also important. “Inflammation causes muscle wasting so wasting is part of the condition,” says Dr Holden. “Exercise can reduce that risk, strengthen your muscles, keep joints mobile and help improve fatigue and pain. It’s also good for your mental health.”
Maintaining a healthy weight and eating a Mediterranean diet with a variety of colorful fruits and vegetables to increase the antioxidants that can reduce inflammation. “Avoid ultra-processed food and sugars and not too much red meat,” says Dr Holden.
Eating oily fish is beneficial – its long-chain omega-3 polyunsaturated fatty acids can reduce inflammation and disease activity in RA. “There is probably a lot more to uncover about diet and RA,” says Dr Holden. “The role of the gut microbiota in maintaining the immune system and inflammatory response is an exciting area of research although we are not there yet.” Finally, don’t smoke! It causes inflammation of the entire body, one of the main causes for arthritis, and also significantly reduces the effectiveness of certain RA medications.
What is the best treatment for RA?
You may be doing all the right things and still have flare-ups – so managing your response and finding a way to live your life to the fullest is key. Trials of CBT for people with RA found that it significantly improved fatigue, mental health and sleep patterns. The program involved people keeping a daily diary of thoughts and feelings, and learning ways to plan and prioritize their days, take regular breaks, notice and manage stressful triggers and break unhelpful thought patterns.
The pain is complicated. It is the body’s response to a threat – and if we are tired, unsupported, lonely, sleep deprived, that threat is greater and our pain response is worse. “This is why tackling sleep problems and stress, and getting support can alleviate physical symptoms,” says Dr Holden.
“You can feel very out of control when you are diagnosed with RA, so learn as much as you can about the condition,” continues Dr. Holden. “Be assertive and get help if you need it.”
Find ways to relieve symptoms that work for you – for example, hot or cold therapy through heat or ice packs, hydrotherapy, physiotherapy, hand splints, cushioned insoles from a podiatrist, a range of home appliances and adaptations that can be made. everyday life easier.
Recommended
Arthritis and joint pain – symptoms to be aware of and how to treat it
Read more