It is hoped that lung cancer could be diagnosed and removed from patients in one sitting in the future thanks to robotics, according to doctors who are trialling the technology.
The method allows doctors to target and remove nodules in the lung with millimeter precision.
Using robotics in this way could be “transformational” for patients and NHS waiting lists, experts have said.
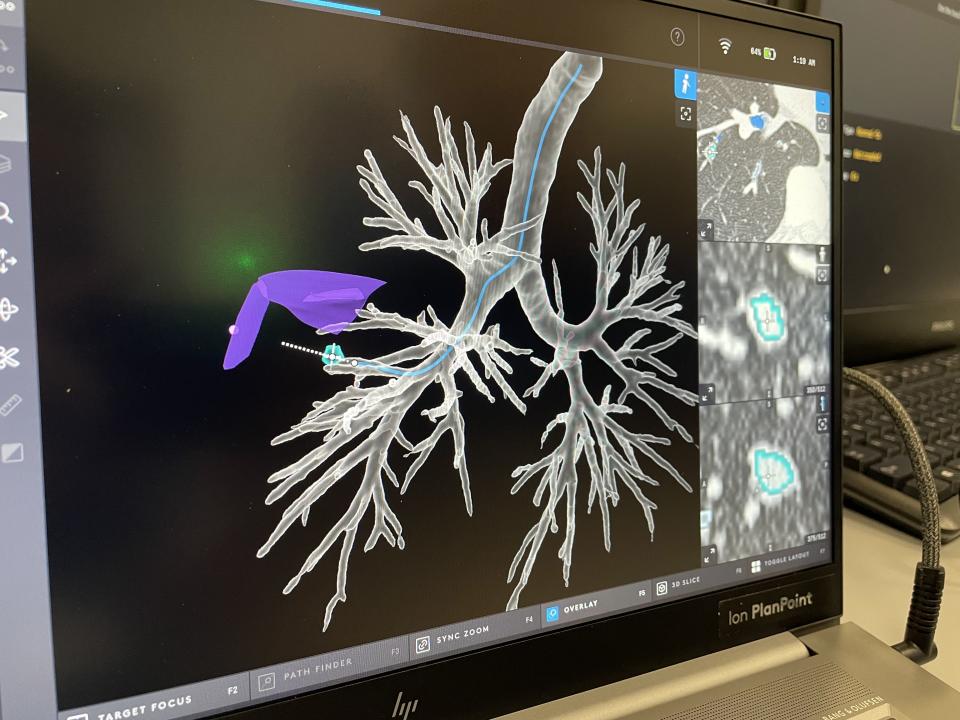
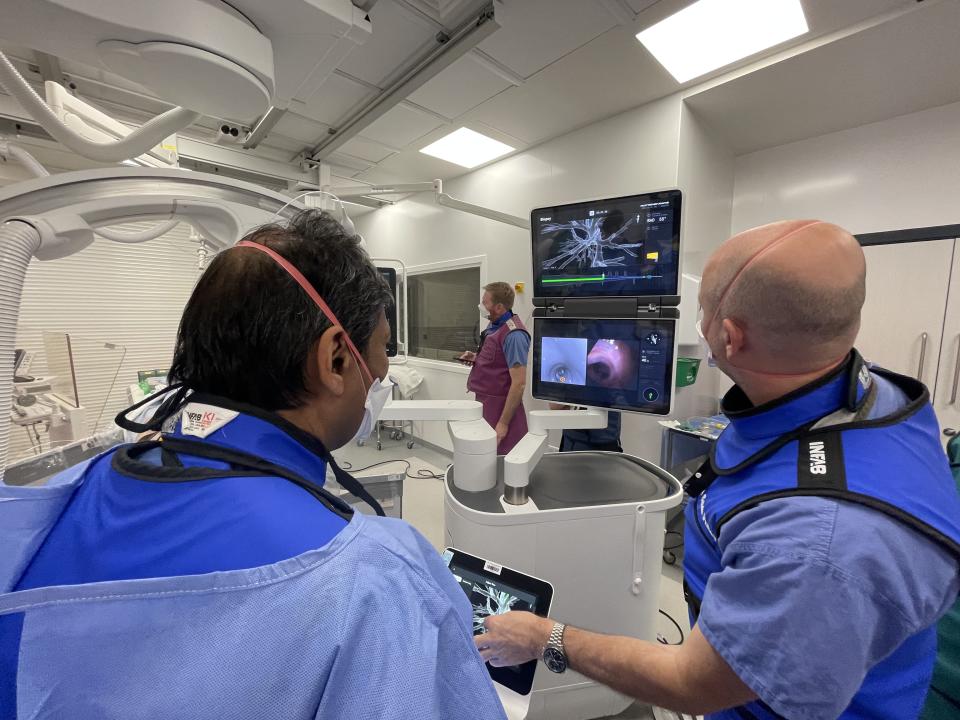
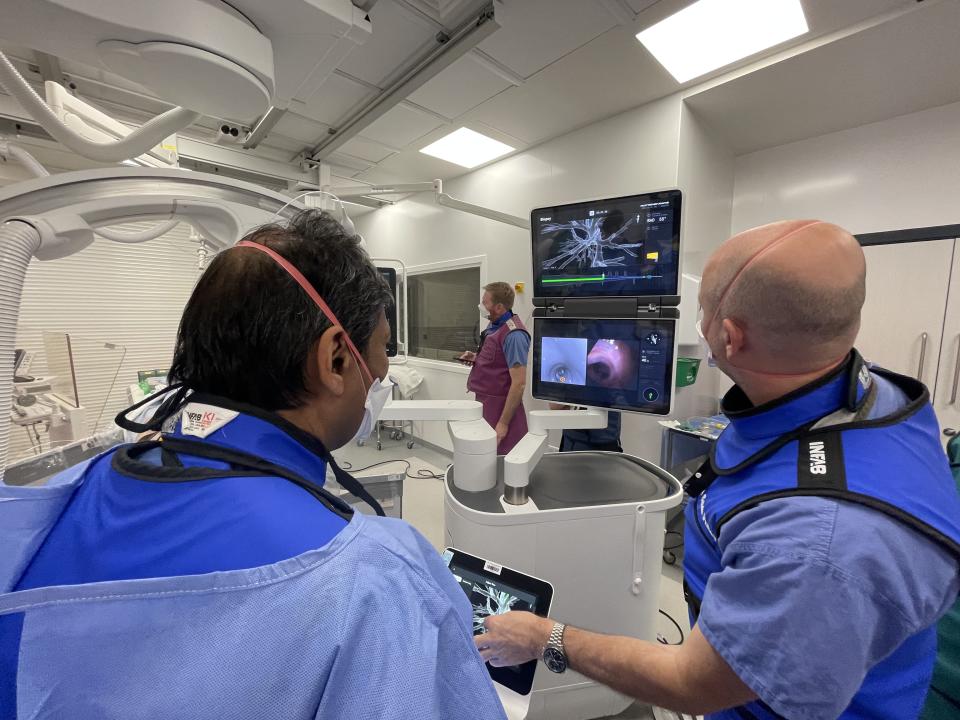
Before the procedure, a CT scan is taken and sent through software to create a detailed 3D road map of the inside of the patient’s lungs from the mouth to the site of the cancer.
A thin robot-guided tube, or catheter, is then placed through the patient’s mouth and into the airways, following this map.
Once located, cancer cells are destroyed using heat in a process called microwave ablation.
Professor Pallav Shah, a consultant respiratory doctor based at the Royal Brompton Hospital in London, told the PA news agency: “We can precisely remove the nodule.
“The first patient we treated was very interesting – she had already had lung cancer and chemotherapy and radiotherapy, but then she developed a place in the field of radiation.
“She could not have more radiotherapy and was not eligible for surgery. We had to be millimeter precise – and we were. She is doing very well now – over six months down the road.”
The team has treated six more patients since then. Professor Shah said: “Generally we are getting good results, but it is early days.”
Current ablation treatments involve having a patient undergo a CT scan to find the cancer and inserting a needle through the skin and directly into the tumor to destroy it.
This may involve multiple ablation attempts, which take “well over an hour, maybe 90 minutes”, according to Professor Shah, and there is a risk of perforating the lung.
The procedure being trialled by Professor Shah and his team takes between 40 and 45 minutes, although the ablation stage only takes three minutes.
Navigational bronchoscopy – where a narrow tube is inserted through the mouth into the airways, allowing doctors to examine nodules – is successful in identifying lung cancer about 65% of the time, according to Professor Shah.
However, the introduction of robotics increases the success rate “significantly”, making it “close to 95%”, he said.
He told PA that “there is a lot of work to be done, but a lot of promise soon” and in the future, he would like to see the diagnosis and treatment of lung cancer at the same sitting.
A current trial aims to treat 32 lung cancer patients who are not suitable or eligible for surgery to determine the safety of the procedure and the rate of cancer recurrence.
The next step is a trial using the method on patients who are eligible for surgery.
One of the biggest comparisons regarding the safety of the new method will be radiotherapy, which works by using radiation to kill cancer cells but has some side effects.
One such side effect is pneumonitis – or inflammation of the lung – which Professor Shah said can be “very predictable and can lead to profound damage and breathlessness”.
According to the NHS, more than 43,000 people are diagnosed with lung cancer in the UK each year. Smoking is the most common cause, accounting for about 70% of cases.
The disease is more likely to be treated successfully if caught early.
Last June, NHS England announced that it would be rolling out its targeted lung health check (TLHC) program in order to detect the disease early and before any symptoms.
People who are eligible for screening are people aged 55 to 74 who are current or former smokers.
“Finding these tumors early is very important,” said Professor Shah. “Usually we only intervene if the node is larger than 10mm or is showing some suspicious changes or growing.
“If it’s between six and 10mm we’d follow up with a scan in three months. But patients don’t like not knowing what it is.
“We don’t want to be overzealous, but we don’t want to waste cancer.”
Creo Medical is a medical device developer that designed the microwave tool used in the procedure.
The company’s chief executive, Craig Gulliford, said: “Combining diagnosis and treatment into one procedure could be game-changing – this reduces the need for the patient to return to a separate, more invasive procedure, which is the standard of care. is currently there.
“By bridging the gap between diagnosis and treatment, it eliminates the long, anxious wait for potential treatment that patients currently face, but it also means that patients can receive treatment before a nodule has time to grow in size or spread to other parts. of the body.
“Currently, there is no early screening for cancer because there are no effective treatments for these early nodules, but this technology can allow earlier treatment, at the point of diagnosis and in a less invasive way, before these nodules. become more serious.”
He added that adopting technology in this way could have “huge benefits” when it comes to reducing NHS waiting lists.
Professor Shah told PA that the adoption of these types of technologies by the NHS was a “complex situation”.
He added: “Robots are going to be expensive, but if you look at the bigger picture you are going to save time.
“If you look at the NHS as a whole, if we can diagnose these tumors early and treat them early, we’ll save a fortune on chemotherapy and radiotherapy.”