A growing number of psychiatrists and psychologists in BC say they are successfully treating patients by harnessing the power of the patients’ own brain waves.
Neurological treatment has been studied for many years but is still a controversial topic among scholars.
“This debate has been going on for a long time,” said Simon Fraser University neuroscientist Randy McIntosh.
“There’s a long history of using things like neurofeedback to help someone rewire their brain.”
McIntosh — a professor in SFU’s department of biomedical physiology and kinesiology, and the BC Leadership Chair in Neuroscience and Technology Transfer Worldwide — said there is evidence that neurofeedback works for patients with certain disorders, even if there is disagreement about exactly how or why.
As with any mental health treatment, however, “There is no one therapy that will work for everyone,” he said.
“But it might work for some.”
‘brain training’
“Neurofeedback is brain training with the goal of increasing cognitive flexibility,” said Victoria psychologist Susan Brock.
Brock, former chair of the Canadian Psychological Association’s quantitative electrophysiology section, said healthy brains “need to be able to switch flexibly between states” of mind at appropriate times.
But conditions like post-traumatic stress disorder (PTSD), one of his specialties, can keep people “in a state of overstimulation even when it’s not necessary.”
Such patients, many of whom are emergency first responders and veterans, cause a loss of cognitive function.


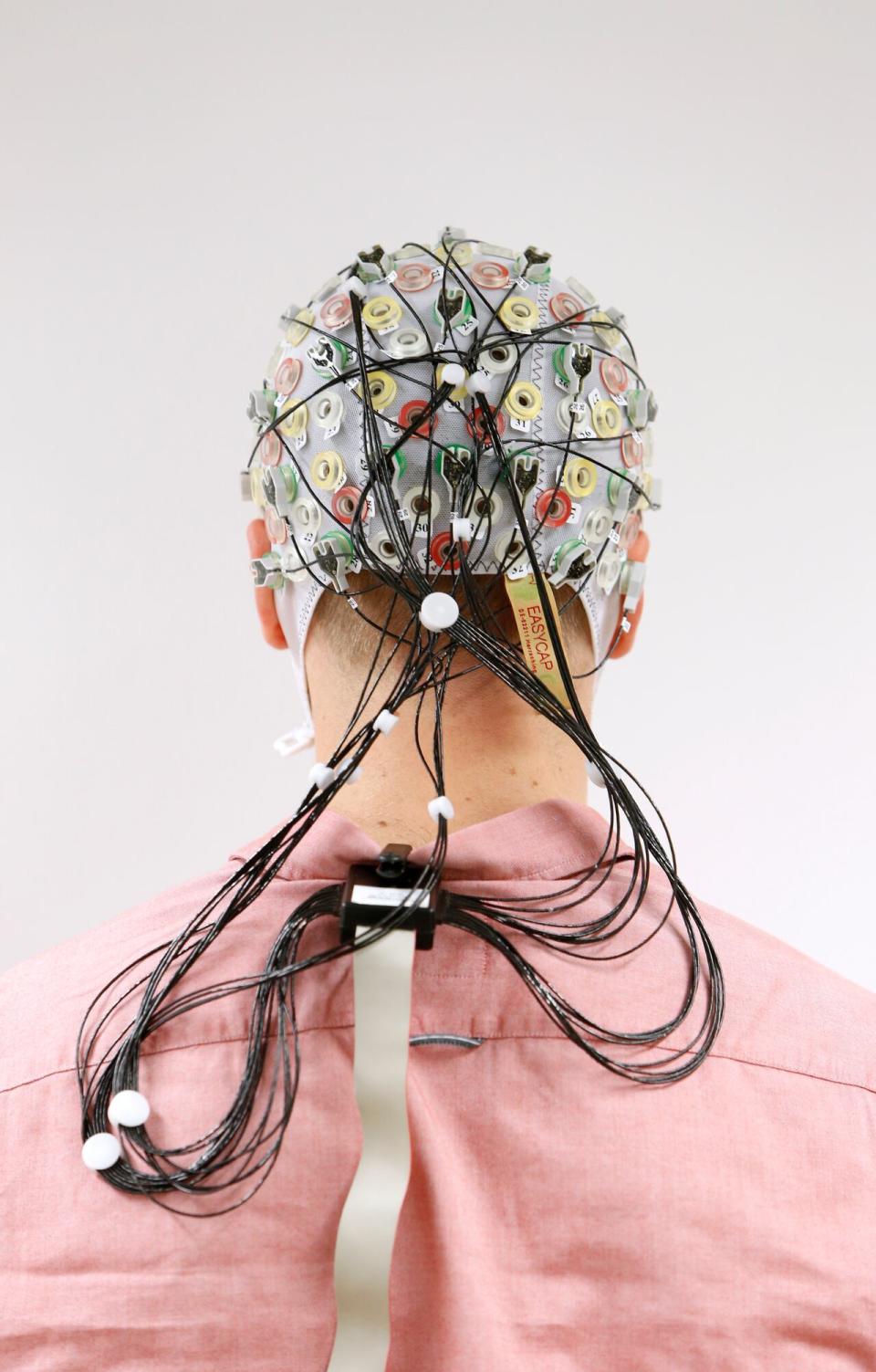
Electroencephalogram-guided neurofeedback involves technicians placing electrodes around a patient’s head, as seen in this photo, to scan the electrical activity in their brain. Here, the patient is seen watching a display monitor. (Craig Chivers/CBC)
A number of private psychiatrists and psychologists throughout BC offer electroencephalography-guided neurofeedback.
The treatment, in simple terms, involves technicians placing electrodes around a patient’s head to scan the electrical activity in their brain, known as an electroencephalogram (EEG).
The EEG creates a sort of computer brain map, which mental health professionals can then use to induce healthier states of mind.
Clinicians use several methods to do this, but most often patients watch a video while fitted with the EEG electrodes.
If their brain shows unhealthy or unwanted electrical activity, the video becomes darker and quieter. But when their brain waves more closely match the “map” of a healthy brain, the video gradually becomes brighter and more audible, as their EEG begins to mirror a healthier or quieter brain.
Basically, being able to enjoy a clearer video acts as a kind of reward or incentive to relax the mind and, as the theory goes, slowly build healthy patterns.
The unorthodox approach is increasingly used among people with a range of mental health conditions from attention deficit hyperactivity disorder (ADHD) to anxiety and post-traumatic stress disorder (PTSD), according to clinicians.
Brock said she has “seen a good response” in her many years of experience using the treatment. She said her patients often report troubling areas of their lives that “haven’t really changed” for the better, despite having previously tried a variety of mental health therapies.
Many still struggled with the ability to change their mind when needed – for example, being able to calm themselves down when distressed.
“It’s not that they don’t want to change,” Brock said. “They don’t know how.
“And for the most part, it’s not for lack of trying; part of the beauty of neurofeedback training is that it happens on a subconscious level.”
More details required
Although frontline psychologists and psychiatrists say they see clear clinical improvements in many of their patients, researchers are divided on the effectiveness of neurofeedback.
Several peer-reviewed studies suggest that better data are needed to prove that it works for the wide range of disorders that practitioners claim to treat. The strongest evidence appears to be for ADHD, anxiety disorders, and traumatic brain injuries.
A Basic and Clinical Neuroscience A 2016 journal article found it to be “a safe and non-invasive procedure that has shown improvement in the treatment of many problems and disorders” including ADHD, anxiety, depression and autism.
But, the authors warned, “its validity has been questioned in terms of inconclusive scientific evidence of its effectiveness.”
Another study, in the journal Psychiatric Clinics in North Americacompared to multiple neuroscience trials, finding that they produced “significant benefits” for ADHD and anxiety and were “probably effective” for traumatic brain injuries and substance use.
But the researchers said “despite the results of positive results” regarding depression and PTSD, the evidence is still “insufficient” without more rigorous or more scientific studies.
It is best to combine it with other treatments
For frontline clinicians, the results are in front of their eyes – and in the experiences of their patients.
Four years ago, psychiatrist Dr. Kourosh Edalati founded Elumind Centers For Brain Excellence, which has private clinics in North Vancouver, Langley and Kelowna. It offers neurofeedback, along with more traditional psychotherapy and medication.
“As an integrated model, we have seen very good responses,” he said. “The principle behind neurofeedback is really operant conditioning … meaning positive and negative reinforcement.
“The brain learns that connecting to the right path is rewarding. Through all the repetition, the brain starts switching to the right paths.”
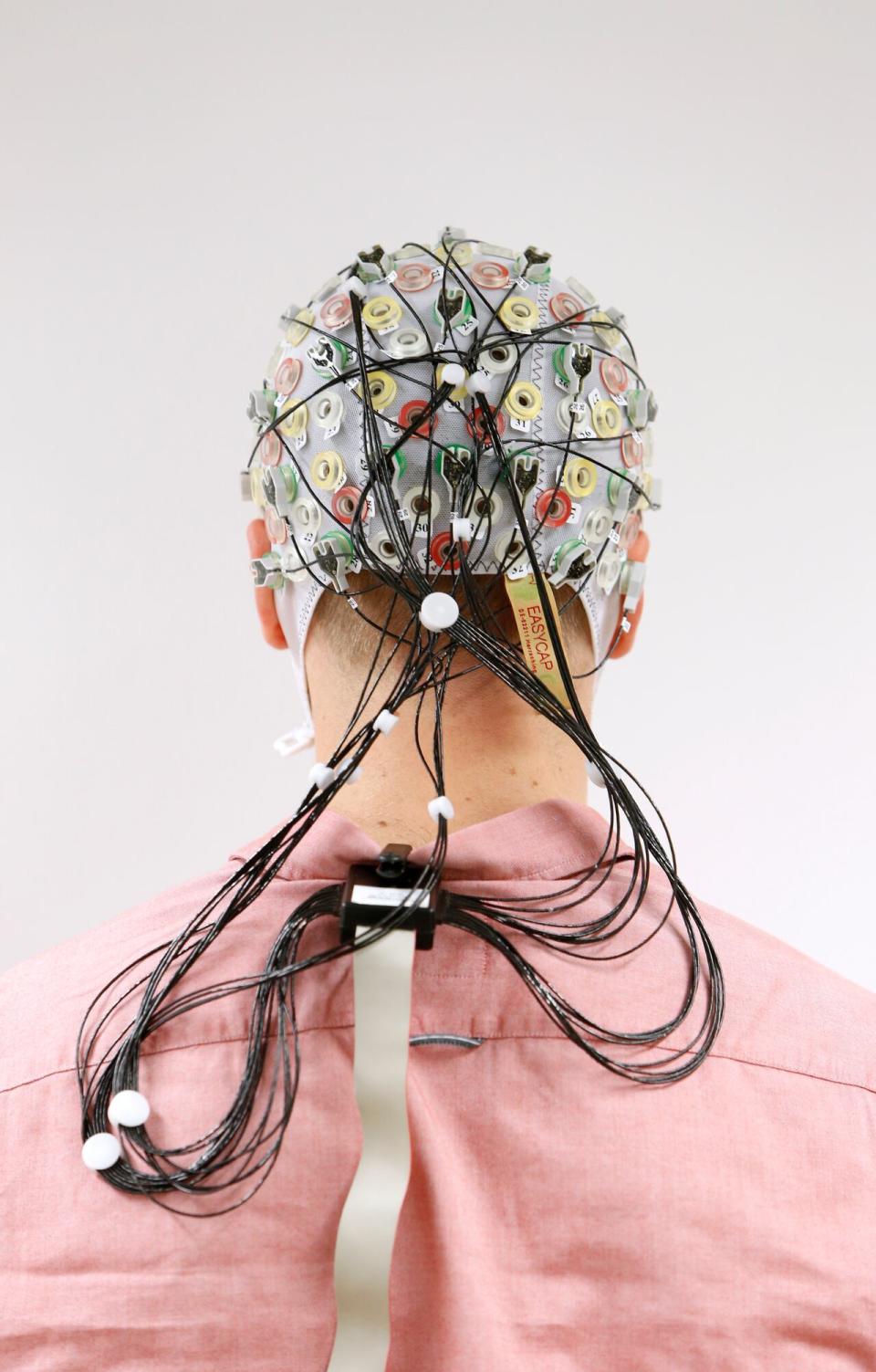
Test subject Niklas Thiel stands with an electroencephalography (EEG) cap that measures brain activity, at the Technische Universitaet Muenchen (TUM) in Garching near Munich in September 2014. (Reuters)
By taking a multifaceted approach to treatment, SFU’s McIntosh said, combining neurofeedback with other methods is probably best.
“We have to be very careful not to think, ‘I’m going to get brain stimulation that will make me better,'” he said. “Some people need extra support.”
“It seems to work for some people … allowing people to get up easily.”
But he said exactly how neurofeedback achieves this in the brain remains unproven.
“Why do these things work?” he said. “The ‘how’ of it is a mystery.
“The evidence is pretty good – but not conclusive.”